Urodynamic Study
Urodynamic studies in concert with an accurate history and physical examination are the most useful clinical tools available for the evaluation of the lower urinary tract and can provide useful clinical information about the function of the urinary bladder, the sphincteric mechanism, and the voiding pattern itself.
Bladder function. This can be evaluated by simple cystometrogram (CMG) that measures vesical pressure as a function of bladder volume. This can provide important information on cystometric bladder capacity, bladder sensation, bladder compliance, and the presence of involuntary bladder contraction and bladder contractility.
Sphincteric function depends on two elements: the smooth muscle sphincter and the voluntary sphincter. The activity of both elements can be recorded urodynamically by measuring urethral pressure profile or by recording sphincter electromyography.
The act of voiding is a function of the interaction between bladder and sphincter, and the result is the flow rate. The flow rate is one major aspect of the total function of the lower urinary tract. It is generally recorded in milliliters per second as well as by total urine volume voided. The simultaneous recording of bladder activity (by intraluminal pressure measurements), sphincteric activity (by electromyography or intraluminal urethral pressure measurements), and flow rate reveals interrelationships among the three elements. Each measurement may give useful information about the normality or abnormality of one specific aspect of lower urinary tract function. A more complete picture is provided by integrating all the three lower tract elements for simultaneous comparison. This comprehensive approach may involve synchronous recordings of variable pressures, flow rate, volume voided, and electrical activity of skeletal musculature around the urinary sphincter (electromyography), along with fluoroscopic imaging of the lower urinary tract. The multiple pressures recorded are quite variable and usually include intravesical pressure, intraurethral pressure at several levels, intra-abdominal pressure, and anal sphincteric pressure as a function of muscular activity of the pelvic floor.
The techniques of urodynamic study must be tailored to the needs of specific patients. Each method has advantages and limitations depending on the requirements of the study. In one patient, results of a single test might be sufficient to establish the diagnosis and suggest appropriate therapy; in another, many more studies might be necessary.
Urodynamic study is an important part of the evaluation of patients with lower urinary tract obstruction, voiding dysfunctions, urinary incontinence, and neuropathic disorders involving the lower urinary tract.
Videourodynamic Study
Fluoroscopy was incorporated with the pressure measurements to adequately assess both anatomy and function.
Urinary Flow Rate
Because urinary flow rate is the product of detrusor action against outlet resistance, a variation from the normal flow rate might reflect dysfunction of either. The normal flow rate from a full bladder is about 20–25 mL/s in men and 25–30 mL/s in women. These variations are directly related to the volume voided and the person's age. Obstruction or detrusor dysfunction should be suspected in any adult voiding with a full bladder at a rate of <15 mL/s. A flow rate <10 mL/s is considered definite evidence of obstruction or detrusor dysfunction. Occasionally, one encounters “supervoiders” with flow rates far above the normal range. This may signify low outlet resistance but is of less concern clinically than obstruction. This phenomenon is more commonly seen in women.
Outlet resistance is the primary determinant of flow rate and varies according to mechanical or functional factors.
Functional, outlet resistance is primarily related to sphincteric activity, which is controlled by both the smooth sphincter and the voluntary sphincter. Overactivity of the smooth sphincter is very rare and essentially nonexistent in females. It is rarely seen in men in association with hypertrophy of the bladder neck due to neurogenic dysfunction or distal obstruction. However, such cases must be evaluated before this conclusion is reached.
On the other hand, increased voluntary sphincteric activity is not uncommon. It is often neglected as a primary underlying cause of increased sphincteric resistance. It is manifested either as lack of relaxation or as actual overactivity during voiding. The normal voluntary sphincter provides adequate resistance, along with the smooth sphincter, to prevent escape of urine from the bladder, but it should completely relax during the act of voiding. If the voluntary sphincter does not relax during detrusor contraction, partial functional obstruction occurs. Overactivity of the sphincter, resulting in increased outlet resistance, is usually a neuropathic phenomenon. However, it can also be functional, resulting from irritative phenomena such as infection or other factors—chemical, bacterial, hormonal, or, even more commonly and often not appreciated, psychological and in patients who are infrequent voiders. This is commonly referred to as pelvic floor dysfunction. This is a spectrum of disease that varies from mild difficulty in voiding associated with incomplete emptying and some pelvic/perineal and genital discomfort to extreme cases of urinary retention known as Fowler's syndrome.
Mechanical factors resulting in obstruction to urine flow are the easiest to identify by conventional methods. In women, they may take the form of large cystoceles, urethral kinks, or, most commonly, iatrogenic scarring, fibrosis, and compression from previous vaginal or periurethral operative procedures. Mechanical factors in men are well known to all urologists; the classic form is benign prostatic hypertrophy. Urethral stricture from various causes and posterior urethral valves are other common causes of urinary obstruction in men, and there are many others.
Normal voiding with a normal flow rate is the product of both detrusor activity and outlet resistance. Complete sphincteric relaxation usually precedes detrusor contraction by a few seconds, and when relaxation is maximal, detrusor activity starts and is sustained until the bladder is empty. A high intravesical pressure resulting from detrusor contraction is usually an indication of increased outlet resistance and is not necessary to initiate normal voiding.
The sequence just described is not essential for normal flow rates. The flow rate may be normal in the absence of any detrusor contraction if sphincteric relaxation is assisted by increased intra-abdominal pressure from straining. Persons with weak outlet resistance and weak sphincteric control can achieve a normal flow rate by complete voluntary sphincteric relaxation without detrusor contraction or straining. A normal flow rate can be achieved in spite of increased sphincteric activity or lack of complete relaxation if detrusor contraction is increased to overcome outlet resistance.
Because a normal flow rate can be achieved in spite of abnormalities of one or more of the mechanisms involved, recording the flow rate alone does not provide insight into the precise mechanisms by which it occurs. Distinction between patterns of flow can be difficult. For practical purposes, if the flow rate is adequate and the recorded pattern and configuration of the flow curve are normal, these variations may not be clinically significant except in rare cases.
The study of urinary flow rate itself is usually called uroflowmetry. The flow rate is generally identified as maximum flow rate, average flow rate, flow time, maximum flow time (the time elapsed before maximum flow rate is reached), and total flow time (the aggregate of flow time if the flow has been interrupted by periods of no voiding) (Figure 29–1). The flow rate pattern is characterized as continuous or intermittent, etc.
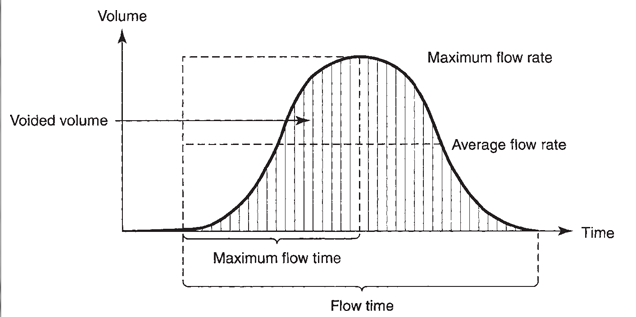
Uroflowmetry. Basic elements of maximum flow, average flow, total flow time, and total volume voided.
Pattern Measurement of Flow Rate
A normal flow pattern is represented by a bell-shaped curve (Figure 29–1). However, the curve is rarely completely smooth; it may vary within limits and still be normal. Flow rate can be determined by measuring a 5 seconds' collection at the peak of flow and dividing the amount obtained by 5 to arrive at the average rate per second. This rough estimate is useful, especially if the flow rate is normal and the values are above 20 mL/s.
In modern practice, the flow rate is more often recorded electronically: The patient voids into a container on top of a measuring device that is connected to a transducer, the weight being converted to volume and recorded on a chart in milliliters per second. Figure 29–2 is an example of such a recording from a normal man. The general bell-shaped curve is quite clear, and the tracing shows all of the values discussed previously: total flow time, maximum flow time, maximum flow rate, average flow rate, and total volume voided. Occasional supervoiders can exceed the limits of the chart, but this is usually not of clinical concern (Figure 29–3). A possible variation in the bell appearance is seen inFigure 29–4.

Classic normal flow rate, with peak of about 30 mL/s and average of about 20 mL/s. On the horizontal scale, one large square equals 5 seconds.

Flow rate of “supervoider.” Maximum flow rate exceeds limits of chart. Tracing shows fast buildup and complete bladder emptying of large volume of urine in a very short period. On the horizontal scale, one large square equals 5 seconds.

Normal flow rate with some variation in appearance of curve. Note the rapid pressure rise but progressive increase to maximum, followed by a sharp drop. There is also fluctuation in ascending limb of tracing. On the horizontal scale, one large square equals 5 seconds.

Rather low flow rate (not exceeding 10 mL/s), yet at one point, the peak reaches 27–32 mL/s. Note again fluctuation in flow. On the horizontal scale, one large square equals 5 seconds.

Very low flow rate of short duration and small volume. Note that maximum flow is not >15 mL/s; however, flow average is <10 mL/s, and flow is almost completely interrupted in the middle. On the horizontal scale, one large square equals 5 seconds.